Sinusitis and its complications

















The paranasal sinuses are air-filled extensions of the nasal cavity. The four paired sinuses – named according to the bone in which they are located – are the maxillary, frontal, sphenoid and ethmoid. Each sinus is lined by a ciliated pseudostratified epithelium, interspersed with mucus-secreting goblet cells.
Acute Sinusitis = Acute inflammation of sinus mucosa
At a glance:
Generally the remit of GP until complications arise
Familiarise yourself with EPOS 2020 guideline flow charts (free on
internet)Hx of URTI, facial pain, nasal obstruction and/or nasal discharge
FNE to confirm presence of pus/oedema in middle meatus
Consider dental abscess if no nasal signs
Sinus X-rays are not necessary
Oral Augmentin and Otrivine nose drops for 1 week and then review
The sinus most commonly involved is the maxillary followed in turn by ethmoid, frontal and sphenoid. Very often, more than one sinus is infected (multisinusitis). Sometimes, all the sinuses of one or both sides are involved simultaneously (pansinusitis unilateral or bilateral).
Causes:
Nasal infections. Sinus mucosa is a continuation of nasal mucosa and infections from nose can travel directly by continuity or by way of submucosal lymphatics. Most common cause of acute sinusitis is viral rhinitis followed by bacterial invasion.
Swimming and diving. Infected water can enter the sinuses through their ostia. High content of chlorine gas in swimming pools can also set up chemical inflammation.
Trauma. Compound fractures or penetrating injuries of sinuses—frontal, maxillary and ethmoid—may permit direct infection of sinus mucosa. Similarly, barotrauma may be followed by infection.
Dental infections. This applies to maxillary sinus. Infection from the molar or premolar teeth or their extraction may be followed by acute sinusitis.
Predisposing factors:
Obstruction to sinus ventilation and drainage. Normally, sinuses are well-ventilated. They also secrete small amount of mucus, which by ciliary movement, is directed towards the sinus ostia from where it drains into the nasal cavity. Any factor(s) which interfere with this function can cause sinusitis due to stasis of secretions in the sinus. They are:
Nasal packing
Deviated septum
Hypertrophic turbinates
Oedema of sinus ostia due to allergy or vasomotor rhinitis
Nasal polypi
Structural abnormality of ethmoidal air cells
Benign or malignant neoplasm.
Stasis of secretions in the nasal cavity - lack of drainage due to viscosity (cystic fibrosis) or obstruction (enlarged adenoids, choanal atresia), and get infected.
Previous attacks of sinusitis. Local defences of sinus mucosa are already damaged.
Environment. Sinusitis is common in cold and wet climate. Atmospheric pollution, smoke, dust and overcrowding also predispose to sinus infection.
Poor general health. Recent attack of exanthematous fever (measles, chickenpox, whooping cough), nutritional deficiencies, systemic disorders (diabetes, immune deficiency syndromes).
Clinical manifestations:
Acute
•Nasal discharge (rhinorrhea)
•Feeling of congestion and obstruction in the nose and face
•Viral infection initially present with bacterial infection soon supervening leading to:
•Purulent rhinorrhea
•Increased congestion with facial pain
•Nasal obstruction
•Pyrexia (in more severe cases)
•Pain radiation:
•Maxillary sinusitis → mainly over the cheeks
•Ethmoidal & frontal sinusitis → periorbital + headache
•Sphenoidal sinusitis → severe deep-seated headache
•Usually more than one sinus is involved (→ pansinusitis)
•Cheek swelling may also indicate a dental abscess [DDx]
•In uncomplicated sinusitis, X-rays are not helpful.
Diagnosis is made clinically.
Treatment:
Simple AS: topical decongestant/ Sinus Rinse (douche)/ analgesia/, topical steroids/oral Abx
Antimicrobial drugs. Ampicillin and amoxicillin are quite effective and cover a wide range of organisms. Erythromycin or doxycycline or cotrimoxazole are equally effective and can be given to those who are sensitive to penicillin. β-lactamase-producing strains of H. influenzae and M. catarrhalis may necessitate the use of amoxicillin/clavulanic acid or cefuroxime axetil. Sparfloxacin is also effective, and has the advantage of single daily dose.
Nasal decongestant drops. 1% ephedrine or 0.1% xylo- or oxymetazoline are used as nasal drops or sprays to decongest sinus ostium and encourage drainage.
Steam inhalation. Steam alone or medicated with menthol or Tr. Benzoin Co. provides symptomatic relief and encourages sinus drainage. Inhalation should be given 15 to 20 minutes after nasal decongestion for better penetration.
Analgesics. Paracetamol or any other suitable analgesic should be given for relief of pain and headache.
Hot fomentation. Local heat to the affected sinus is often soothing and helps in the resolution of inflammation.
Complicated AS: IV ABX + CT Scan (paranasal sinuses + Brain) +/- surgery (e.g. antral lavage; depends on clinical scenario).
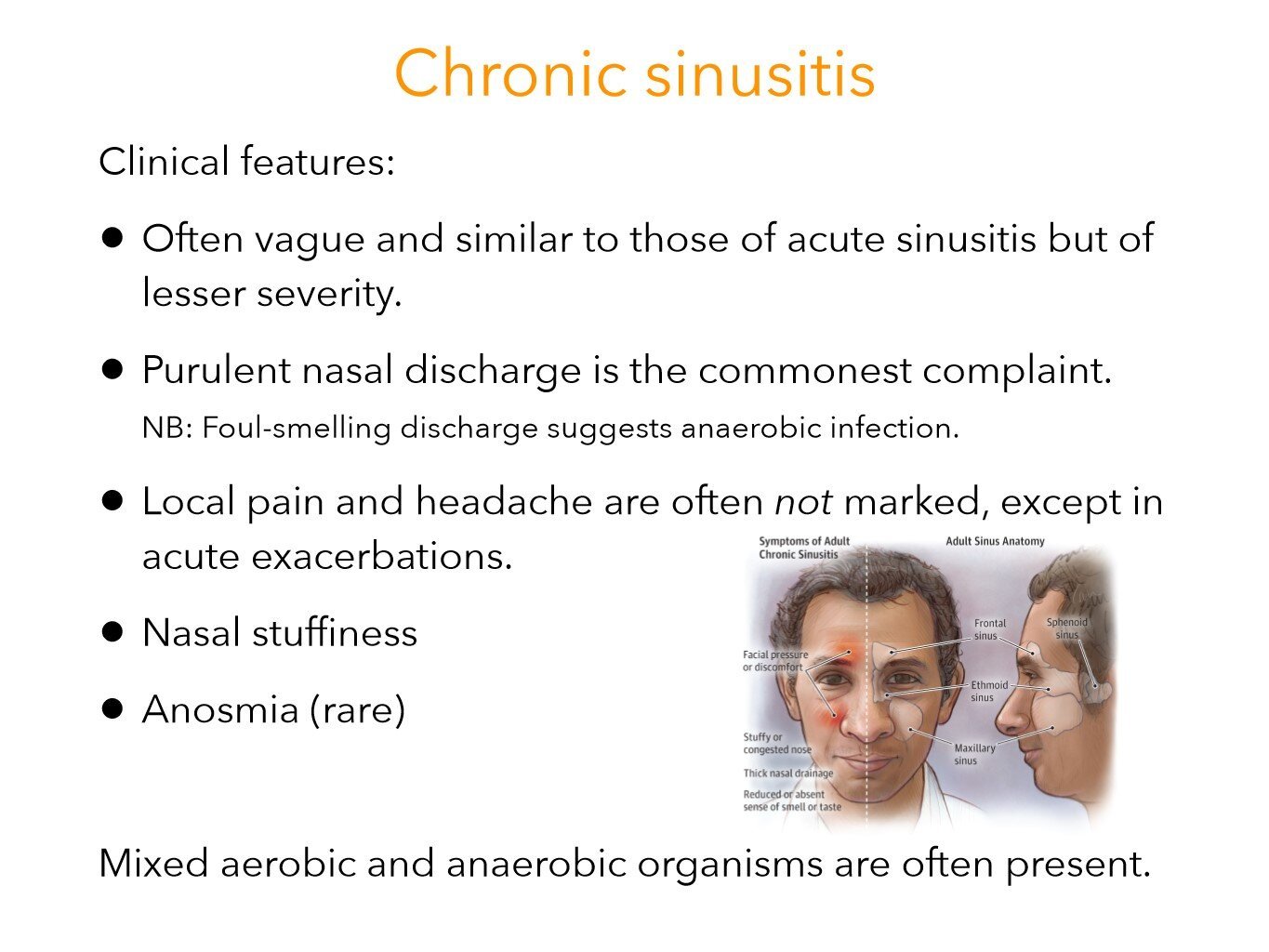
Chronic sinusitis
Can be with or without nasal polyps (polyp is insensitive, whereas the conchae are tender to touch)
Previous acute rhinosinusitis failing to resolve
Constant nasal mucopurulent discharge, congestion and facial pain
Anosmia/hyposmia with nasal obstruction are common
Pathophysiology
Acute infection destroys normal ciliated epithelium impairing drainage from the sinus. Pooling and stagnation of secretions in the sinus invites infection. Persistence of infection causes mucosal changes, such as loss of cilia, oedema and polyp formation, thus continuing the vicious cycle.
Treatment:
Conservative measures - antibiotics, decongestants, antihistamines and sinus irrigations.
Endoscopic sinus surgery - to provide free drainage and ventilation
Radical surgery - to remove all irreversible diseases so as to provide wide drainage or to obliterate the sinus.
Periorbital cellulitis
This is a sight and life threatening emergency. Infection can spread from the ethmoids through the lamina papyracea into the orbit then on into the cavernous sinus.
This needs urgent review and input from ENT, ophthalmology and paediatrics (as the patients are usually children)
Give IV Abx as per protocol, check visual acuity and eye movements
If the patient has eye signs, after discussing with reg, organise urgent
CT sinuses to exclude subperiosteal abscess which may lead to
blindness if not urgently surgically drained.Obtain ophthalmology review urgently
If child also involve paediatricians
Ensure all complicated sinusitis patients are discussed with the on call
SpRIf the patient does not improve after 24-48 hours they will likely need a
CT
Intracranial infection
Meningitis, extradural and subdural abscesses
Neurological emergencies
Cerebral abscesses (frontal lobe) often have an insidious development.
Suspect if headache, drowsy or confused
Request urgent CT/MRI brain with contrast and contact neurosurgery for review
Beware paediatric patients with recent frontal sinus infection being apathetic or exhibiting abnormal behaviour
Non-surgical management
Broad spectrum IV antibiotics - consult your local microbiology guidance
Nasal decongestants
Steroid nasal drops
Nasal douches
Supportive: IV fluids, analgesia
Further management
You will need senior input for the following:
Surgical drainage of intraorbital collection:
External-approach drainage (via Lynch-Howarth incision if medial). The most reliable approach in a compromised eye or where access is challenging (e.g. young children).
Endoscopic approach via an ethmoidectomy.
Further imaging may be indicated if the patient fails to progress on medical treatment for 24-36 hours, or if a procedure fails to result in significant improvement.
Pott’s puffy tumor = osteomyelitis of the frontal bone with associated subperiosteal abscess causing swelling and edema over the forehead and scalp.
Management: Broad-spectrum antibiotics for 4 to 6 weeks, along with surgical drainage.
Sources:
Dhingra, P. L. Diseases of Ear, Nose and Throat. Elsevier, 2010
Corbridge, Rogan, and Nicholas Steventon. Oxford Handbook of ENT and Head and Neck Surgery. 3rd ed., Oxford University Press, 2020.
Ludman, Harold S., and Patrick J. Bradley. ABC of Ear, Nose and Throat. 6th ed., Wiley, 2013.
Corbridge, Rogan J. Essential ENT. 2nd ed., CRC Press, 2011.
A diagram illustrating the subtle differences between acute and chronic sinusitis

