Parathyroid Pathology










Anatomy
· Usually there are 4 parathyroid glands, most often located behind the thyroid gland.
· Ectopic thyroid glands can also be found in the mediastinum, under the jaw, retro-tracheal, retro-sternal
· Usually the size of a grain of rice with a characteristic yellow/golden colour
· Blood supply is usually solely supplied by the inferior thyroid artery (hence care must be taken in surgery to not ligate both)
Function
· The sole purpose of parathyroid hormone is to regulate calcium levels in the body, calcium is the most tightly controlled element in the body since it has its own hormonal system purely for regulation.
· Parathyroid glands produce parathyroid hormone (PTH), which has a very low half-life of approximately 5 minutes.
· PTH is secreted in response to hypocalcaemia
· PTH is inhibited by hypercalcaemia via a negative feedback loop
(Hypercalcaemia also causes the parafollicular cells of the thyroid gland to secrete Calcitonin which also helps to reduce Calcium levels)
Actions of PTH:
-Leads to an increased in calcium but also a NET REDUCTION in Phosphate levels
· Increases absorption of Ca2+ in the gut / Increased absorption of phosphate in the gut
· Increase re-absorption Ca2+ in kidney / Reduce re-absorption of Phosphate
· Increased indirect osteoclastic activity on bones (releases both Calcium & Phosphate)
· Increased activation of Vitamin D
-PTH action on osteoclasts is indirect, since osteoblasts do not have a receptor for PTH. Instead, PTH binds to receptors on osteoblasts which then express RANKL receptors resulting in osteoclast activation.
Hyperparathyroidism
· Usual onset is age 50-60
· X3 more common in females
· Lifetime incidence of 1 in 80 (>1%)
Classification:
1) Primary
· Adenoma – Autonomous abnormal secretion. 80% is due to a parathyroid adenoma, most other causes are due to several adenomas. This . can only be cured with surgery
· Hyperplasia – all 4 glands enlarged – usually due to Multiple Endocrine Neoplasia (MEN) syndromes
· Parathyroid cancer is extremely rare
2) Secondary (Physiological)
· Occurs as a physiological response to hypocalcaemia
· Most often caused by renal failure
· Can also be caused by Vitamin D deficiency
3) Tertiary
· Hyperplasia due to long-term secondary hyperparathyroidism
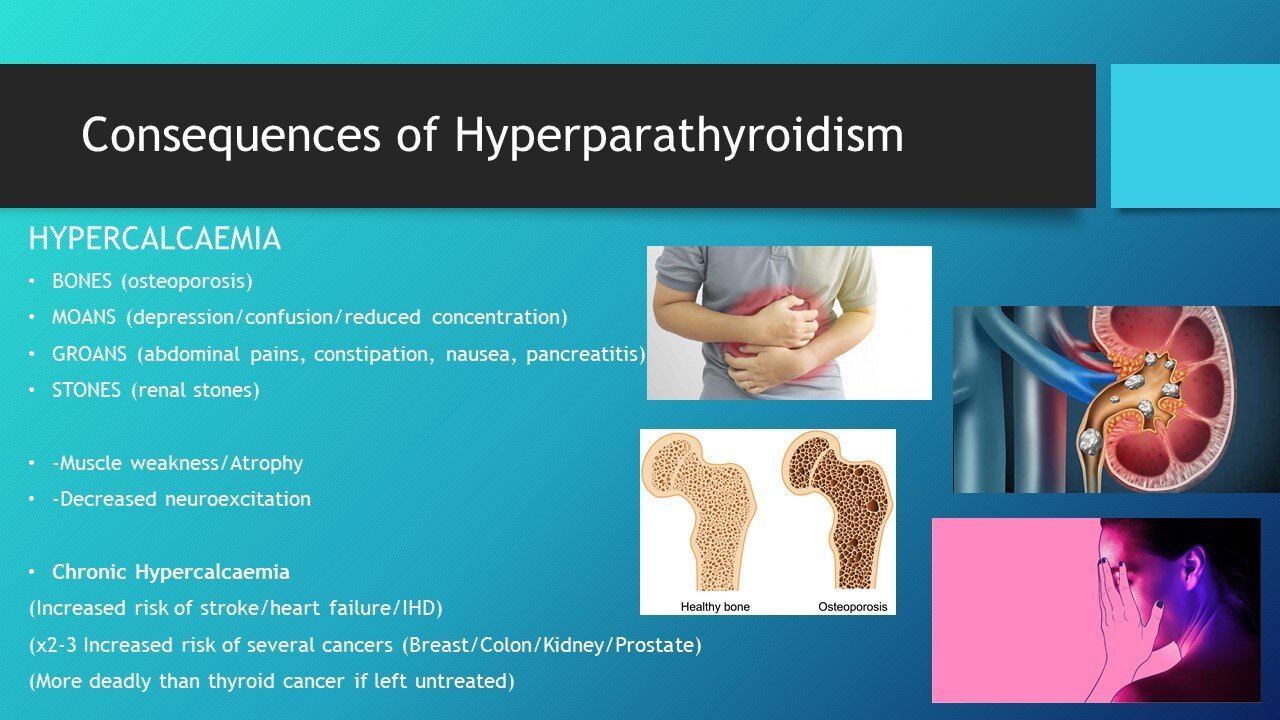
Consequences of Hyperparathyroidism
HYPERCALCAEMIA
· BONES (osteoporosis)
· MOANS (depression/confusion/reduced concentration)
· GROANS (abdominal pains, constipation, nausea)
· STONES (renal stones)
Calcium is the primary element that causes muscles to contract but is also involved with the electrical transmission with nerves. This explains lots of the side effects that can come from deranged levels of Calcium (low mood, abdominal pains, muscle twitching)
· Chronic hypercalcaemia can lead to an increased risk of stroke/heart failure/ischaemic heart disease
· Parathyroid cancer is extremely rare but chronic hypercalcaemia can lead to an x2-3 increased risk of several cancers (breast/colon/kidney/prostate)
Parathyroid adenomas
· Benign tumour (overproducing PTH) – it has lost its regulatory mechanisms
· 70% - one adenoma, 30% - >1
· 10% are ectopic
· To be curative will need to remove all adenomas
-75% of people with primary hyperparathyroidism are asymptomatic (don’t have stones/ GI upsets etc but likely manifest more subtle psychological effects impacting on the quality of life etc)
Diagnosis:
-Often incidental hypercalcaemia
-Raised PTH on bloods (often 50-150)
-Renal stones/Bone #’s
Imaging:
-Sestamibi parathyroid scintigraphy (nuclear imaging) – can be useful to help locate parathyroid tissue (only picks up approx. 50% of adenomas so is not diagnostic but can help exclude the presence of ectopic adenomas)
-USS (user dependant) (sensitivity ranging from 25% to 75% depending on the experience of the user)
Indications for parathyroidectomy
· Symptomatic hyperparathyroidism
· Asymptomatic with:
-24 hour calcium > 400mg
Serum Calcium >1mg/dl over the normal limit
-Age <50
-Bone density > 2.5 SD’s from peak
-Creatinine clearance >30% below normal for the patient
Complications of parathyroidectomy
• Hypocalcaemia
Transient – time delay for remaining parathyroid tissue to compensate or damage to blood supply – Inferior thyroid artery
Permanent – Accidental removal of all 4 glands (<1% by experienced ENT surgeons)
• Damage to surrounding structures (RLN, other parathyroid tissues, blood vessels)
• (1-2% damage to RLN by experienced ENT surgeons, 3-4% if not doing routine parathyroid surgery)
• Unable to locate adenoma
• Unable to locate an additional adenoma
Steps that can be taken to reduce complications:
• NERVE MONITORS
• INTRA-OPERATIVE PTH
• USUALLY ROUTINE TO IDENTIFY ALL 4 GLANDS
• LEAVE SOME PARATHYROID TISSUE BEHIND
Post parathyroidectomy management:
• Observe for acute hypocalcaemia (regular blood checks)
• Symptoms of tingling, confusion, cramps (This can be normal post successful parathyroidectomy)
TREATMENT – More Calcium (will likely be transient)
• Patients often given calcium replacement for the first few weeks post-surgery
(Can take a few weeks for the normal glands to upregulate activity (“switch back on”)
