Deep Neck Space Infections




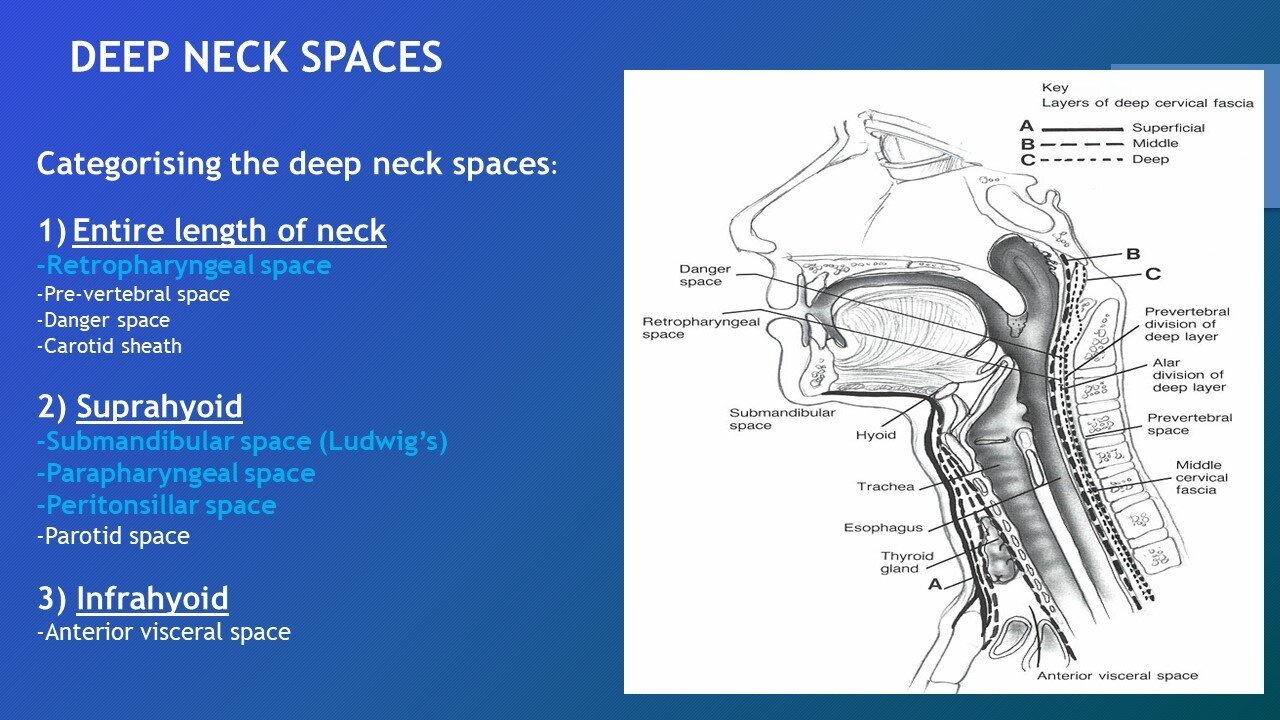

















The neck is divided in to separate compartments, these are further divided by layers of fascia
These deep neck space compartments act as spaces for the spread of infection and tumours
Deep neck spaces carry a risk of mortality of 1-2%
Layers of cervical fascia
Cervical fascia can be divided into superficial and deep fascia.
The superficial fascia consists of the dermis, subcutaneous tissue and platysma.
The deep fascia is further subdivided into superficial, middle and deep layers.
Superficial/investing layer of deep fascia covers the parotid glands as well as muscles deep to the platysma
Middle (Pre-tracheal) fascia – encloses visceral organs (thyroid/parathyroid/larynx/trachea)
Deep (prevertebral layer) – Covers vertebral column and prevertebral muscles
Clinical features
Odynophagia (pain on swallowing)
Dysphagia (difficulty swallowing)
Restricted neck movements
Trismus
Voice change
Respiratory distress/Stridor
Neck swellings
Fevers/septic
Raised inflammatory markers on bloods
Flexible nasendoscopy findings (Airway compromise? Parapharyngeal swelling? Posterior pharyngeal wall swelling?)
Management
ABC
Involve seniors early (ENT/ITU)
Secure airway if needed
High flow oxygen
FNE if stable enough
Bloods (including cultures)
IV Abx (Follow trust guidelines)
IV Dexamethasone (7.6mg)
PRN adrenaline nebs if needed
Imaging (CT neck + chest with contrast) – D/W Senior
Surgical drainage
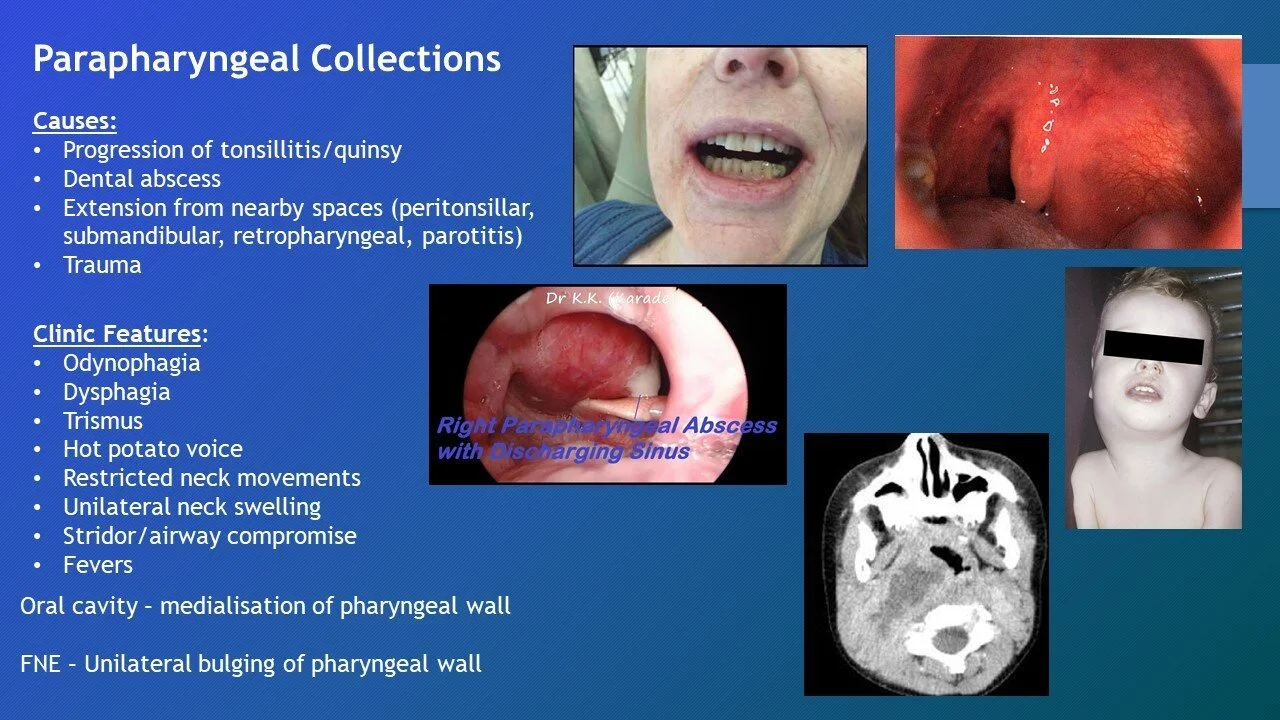
Parapharyngeal Infections
Upside down pyramid
Base: Skull Base
Apex: Hyoid
Lateral: Ramus of mandible, medial pterygoid, deep lobe of parotid
Medial: Bucco-pharyngeal fascia
Causes:
Progression of tonsillitis/quinsy (most common)
Dental abscess
Extension from nearby spaces (peritonsillar, submandibular, retropharyngeal, parotitis)
Trauma
FNE may show a unilateral swelling of the pharyngeal wall (See the presentation for examples)
Complications:
Neurological (CN 9-12 palsies?)
Septic internal jugular vein thrombosis
Horner’s syndrome
Airway compromise
Carotid artery erosion
Extension to other spaces (mediastinum)
Retropharyngeal infections
More common in younger patients (96% occur before 6 years of age)
Common causes:
Preceding URTI (tonsillitis/sinusitis/quinsy)
Trauma (More common cause in adults
Extension from other spaces (e.g: parapharyngeal)
Diagnosis and treatment as above
FNE may show swelling of the posterior pharyngeal wall (See the presentation for examples)
Submandibular Infections (Ludwig’s angina)
Subdivisions:
Sublingual space – Above mylohyoid
Submaxillary space – Below mylohyoid
What is it?
Rapidly spreading cellulitis of the floor of the mouth (submandibular space)
Life-threatening airway risk (URGENT)
Causes?
Dental infection (80%)
Injury to the floor of the mouth
Submandibular sialadenitis
Clinical features?
Raised hard floor of the mouth
Elevated oedematous tongue
“Double tongue sign”
Airway compromise
Trismus
Drooling
Peritonsillar Collection (Quinsy)
Abscess formation between the capsule of the tonsil and the pharyngeal muscles
Usually a consequence of acute tonsillitis
Complications:
Parapharyngeal abscess
Retropharyngeal abscess
Internal jugular vein thrombosis
Septicaemia
Diagram of deep neck spaces

